Research
Therapy Recommendations
Project 1. Personalized Neoadjuvant Therapy Recommendations in Breast Cancer from an Explainable Multi-Omics Response Model
Background
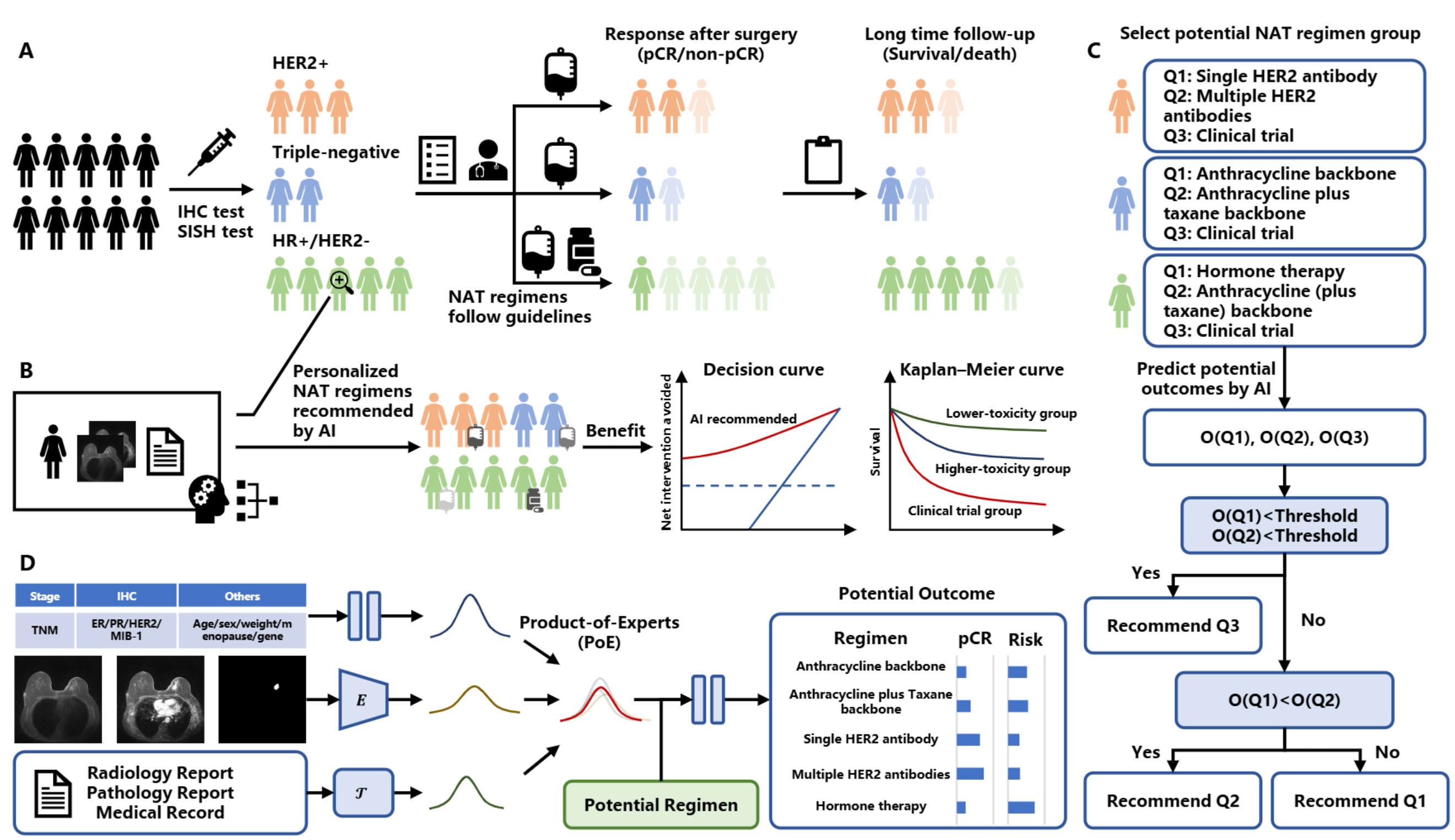
The neoadjuvant therapy (NAT) regimen for breast cancer is generally determined according to cancer stage and molecular subtypes without fully considering the intra-individual variability within patients, which may lead to inefficiency or overtreatment with associated toxicities and side effects. Artificial intelligence may achieve personalized regimen recommendations by learning the synergistic relationship between the pre-NAT individual-patient data, regimens, and the corresponding short- or long-term therapy response.
Methods
In this retrospective study, we collected patients with breast cancer who were treated with NAT from the Netherlands and the USA. We developed and externally validated a multi-omics model that incorporates pre-treatment clinical data, DCE-MRI images, and medical reports. This model can establish the likelihood of a particular treatment leading to a specific response, and it uses the joint distribution from multiple modalities to predict pathologic complete response (pCR) and risk scores of the treatment. We subsequently evaluated the potential benefit to patients receiving a personalized regimen recommended based on the predicted pCR and risk scores.
Results
We trained our model on 655 patients and evaluated it on an independent validation cohort of 655 patients and an external validation cohort of 241 patients. Given the factual regimens, we found that the model can correctly predict the corresponding therapy response, with AUC of 0.80 (95% CI 0.73-0.87), 0.75 (95% CI 0.66-0.83), and 0.85 (95% CI 0.77-0.92) for pCR prediction of HER2+, triple-negative, and ER/PR+\&HER2- patients in the independent validation cohorts, respectively. Patients in the high-risk group had a worse prognosis compared to the low-risk group, as demonstrated by a hazard ratio (HR) of 3.29 (95% CI 0.91-11.94), 3.54 (95% CI 1.52-8.20), and 2.78 (95% CI 1.45-5.31) for overall survival of patients in the different molecular subtypes. We compared the model-predicted pCR and risk scores of the same patient treated with different potential NAT regimens and predicted potentially more effective regimens. Results show that the model can potentially recommend transiting patients with better prognoses to lower-toxicity regimens, and patients with worse prognoses to higher-toxicity regimens or clinical trials.